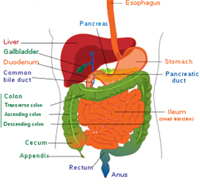
Gastrointestinal Surgery is an umbrella term for all operations on the gastrointestinal tract. In this age of specialization,it is broadly divided into Upper Gastrointestinal surgery and Colorectal surgery
Surgery is often the main treatment for earlier stage colon cancers.
 A colectomy (sometimes called a hemicolectomy, partial colectomy, or segmental resection) removes part of the colon, as well as nearby lymph nodes. The surgery is referred to as an open colectomy if it is done through a single incision in the abdomen.The day before surgery, you will most likely be told to completely empty your bowel. This is done with a bowel preparation, which may consist of laxatives and enemas. Just before the surgery, you will be given general anesthesia, which puts you into a deep sleep.
A colectomy (sometimes called a hemicolectomy, partial colectomy, or segmental resection) removes part of the colon, as well as nearby lymph nodes. The surgery is referred to as an open colectomy if it is done through a single incision in the abdomen.The day before surgery, you will most likely be told to completely empty your bowel. This is done with a bowel preparation, which may consist of laxatives and enemas. Just before the surgery, you will be given general anesthesia, which puts you into a deep sleep.
During the surgery, your surgeon will make an incision in your abdomen. He or she will remove the part of the colon with the cancer and a small segment of normal colon on either side of the cancer. Usually, about one-fourth to one-third of your colon is removed, but more or less may be removed depending on the exact size and location of the cancer. The remaining sections of your colon are then reattached. Nearby lymph nodes are removed at this time as well. Most experts feel that taking out as many nearby lymph nodes as possible is important, but at least 12 should be removed.
When you wake up after surgery, you will have some pain and probably will need pain medicines for 2 or 3 days. For the first couple of days, you will be given intravenous (IV) fluids. During this time you may not be able to eat or you may be allowed limited liquids, as the colon needs some time to recover. But a colon resection rarely causes any major problems with digestive functions, and you should be able to eat solid food again in a few days.
It's important that you are as healthy as possible for this type of major surgery, but in some cases an operation may need to be done right away. If the tumor is large and has blocked your colon, it may be possible for the doctor to use a colonoscope to put a stent (a hollow metal or plastic tube) inside the colon to keep it open and relieve the blockage for a short time and help prepare for surgery a few days later.
If a stent can't be placed or if the tumor has caused a hole in the colon, surgery may be needed right away. This usually is the same type of operation that's done to remove the cancer, but instead of reconnecting the segments of the colon, the top end of the colon is attached to an opening (stoma) in the skin of the abdomen to allow body wastes out. This is known as a colostomy and is usually temporary. Sometimes the end of the small intestine (the ileum) is connected to a stoma in the skin instead. This is called an ileostomy. A removable collecting bag is connected to the stoma to hold the waste. Once you are healthier, another operation (known as a colostomy reversal or ileostomy reversal) can be done to attach the ends of the colon back together or to attach the ileum to the colon. Rarely, if a tumor can't be removed or a stent placed, the colostomy or ileostomy may need to be permanent.
This newer approach to removing part of the colon and nearby lymph nodes may be an option for some earlier stage cancers. Instead of making one long incision in the abdomen, the surgeon makes several smaller incisions. Special long instruments are inserted through these incisions to remove part of the colon and lymph nodes. One of the instruments has a small video camera on the end, which allows the surgeon to see inside the abdomen. Once the diseased part of the colon has been freed, one of the incisions is made larger to allow for its removal.
This type of operation requires the same type of preparation before surgery and the same type of anesthesia during surgery as an open colectomy (see above).
Because the incisions are smaller than with an open colectomy, patients may recover slightly faster and have less pain than they do after standard colon surgery.
Laparoscopic-assisted surgery is as likely to be curative as the open approach for colon cancers. But the surgery requires special expertise. If you are considering this approach, be sure to look for a skilled surgeon who has done many of these operations.
Some early colon cancers (stage 0 and some early stage I tumors) or polyps can be removed by surgery through a colonoscope. When this is done, the surgeon does not have to cut into the abdomen. For a polypectomy, the cancer is removed as part of the polyp, which is cut at its stalk (the area that resembles the stem of a mushroom). Local excision removes superficial cancers and a small amount of nearby tissue.
Surgery is usually the main treatment for rectal cancer, although radiation and chemotherapy will often be given before or after surgery. Several surgical methods can be used for removing or destroying rectal cancers.
These procedures, described in the colon surgery section, can be used to remove superficial cancers or polyps. They are done with instruments inserted through the anus, without making a surgical opening in the skin of the abdomen.
As with polypectomy and local excision, local transanal resection (also known as transanal excision) is done with instruments inserted through the anus, without making an opening in the skin of the abdomen. This operation cuts through all layers of the rectum to remove cancer as well as some surrounding normal rectal tissue, and then closes the hole in the rectal wall. This procedure can be used to remove some T1 N0 M0 stage I rectal cancers that are relatively small and not too far from the anus. It is usually done with local anesthesia (numbing medicine) -- you are not asleep during the operation.
This operation can sometimes be used for early T1 N0 M0 stage I cancers that are higher in the rectum than could be reached using the standard transanal resection (see above). A specially designed magnifying scope is inserted through the anus and into the rectum, allowing the surgeon to do a transanal resection with great precision and accuracy. This operation is only done at certain centers, as it requires special equipment and surgeons with special training and experience.
Some stage I rectal cancers and most stage II or III cancers in the upper third of the rectum (close to where it connects with the colon) can be removed by low anterior resection. In this operation, the part of the rectum containing the tumor is removed without affecting the anus. The colon is then attached to the remaining part of the rectum so that after the surgery, you will move your bowels in the usual way.
A low anterior resection is like most abdominal operations. You will most likely be instructed to take laxatives and enemas before surgery to completely clean out the intestines. Just before surgery, you will be given general anesthesia, which puts you into a deep sleep. The surgeon makes an incision in the abdomen. Then the surgeon removes the cancer and a margin of normal tissue on either side of the cancer, along with nearby lymph nodes and fatty and fibrous tissue around the rectum. The colon is then reattached to the rectum that is remaining so that a permanent colostomy is not necessary. If radiation and chemotherapy have been given before surgery, it is common for a temporary ileostomy to be made (where the last part of the small intestine -- the ileum -- is brought out through a hole in the abdominal wall). Usually this can be reversed (the intestines reconnected) about 8 weeks later.
The usual hospital stay for a low anterior resection is 4 to 7 days, depending on your overall health. Recovery time at home may be 3 to 6 weeks.
Some stage I and most stage II and III rectal cancers in the middle and lower third of the rectum require removing the entire rectum (proctectomy). The colon is then connected to the anus (colo-anal anastomosis). The rectum has to be removed to do a total mesorectal excision (TME), which is required to remove all of the lymph nodes near the rectum. This is a harder procedure to do, but modern techniques have made it possible.
Sometimes when a colo-anal anastomosis is done, a small pouch is made by doubling back a short segment of colon (colonic J-pouch) or by enlarging a segment (coloplasty). This small reservoir of colon then functions as a storage space for fecal matter like the rectum did before surgery. When special techniques are needed to avoid a permanent colostomy, you may need to have a temporary ileostomy opening for about 8 weeks while the bowel heals. A second operation is then done to reconnect the intestines and close the ileostomy opening.
This operation requires general anesthesia (where you are asleep). The usual hospital stay for a colo-anal anastomosis, like a low anterior resection, is 4 to 7 days, depending on your overall health. Recovery time at home may be 3 to 6 weeks.
This operation is more involved than a low anterior resection. It can be used to treat some stage I cancers and many stage II or III rectal cancers in the lower third of the rectum (the part nearest to the anus), especially if the cancer is growing into the sphincter muscle (the muscle that keeps the anus closed and prevents stool leakage).
Here, the surgeon makes one incision in the abdomen, and another in the perineal area around the anus. This incision allows the surgeon to remove the anus and the tissues surrounding it, including the sphincter muscle. Because the anus is removed, you will need a permanent colostomy to allow stool a path out of the body.
This operation requires general anesthesia (where you are asleep). As with a low anterior resection or a colo-anal anastomosis, the usual hospital stay for an AP resection is 4 to 7 days, depending on your overall health. Recovery time at home may be 3 to 6 weeks.
If the rectal cancer is growing into nearby organs, a pelvic exenteration may be recommended. This is an extensive operation. Not only will the surgeon remove the rectum, but also nearby organs such as the bladder, prostate (in men), or uterus (in women) if the cancer has spread to these organs. You will need a colostomy after pelvic exenteration. If the bladder is removed, you will also need a urostomy(opening where urine exits the front of the abdomen and is held in a portable pouch).
Operation on Piles Unique technique of Sclerotherapy with Closed Hemorrhoidectomy .Injection of a sclerosant solution at the apex of the Piles ; No patient has come back with recurrence by this technique .
Operation for Fissure in Ano:
FissurectomyBoth these clinical problems are operated under regional or General Anesthesia and as a Day Care Procedure , Early return to normal activity , No discomfort in sitting or walking ,No dressings required , No stitching or Stapling done in this technique.
Operation for Fistula in Ano : Fistulectomy for Simple and Complex Fistula in Ano .


.jpg)