Gastrointestinal Surgery is an umbrella term for all operations on the gastrointestinal tract. In this age of specialization,it is broadly divided into Upper Gastrointestinal surgery,Colorectal surgery and Hepatobiliary - Pancreatic surgery.
Achalasia is primarily a disorder of motility of the lower oesophageal or cardiac sphincter. The smooth muscle layer of the oesophagus has impaired peristalsis and failure of the sphincter to relax causes a functional stenosis or functional oesophageal stricture. Most cases have no known underlying cause, but a small proportion occur secondary to other conditions, e.g. oesophageal cancer.
Occurs due to Acid and Alkali Ingestion accidentally or suicidal tendency by the patient .Treatment involves major surgery like Coloplasty Operation ,which can be done in two different approaches giving a new conduit for the food passage .
There are two main types of esophageal cancer. Both types are diagnosed, treated, and managed in similar ways.Adenocarcinoma of the esophagus: This type is usually found in the lower part of the esophagus, near the stomach. In the United States, adenocarcinoma is the most common type of esophageal cancer. It's been increasing since the 1970s.
Squamous cell carcinoma of the esophagus: This type is usually found in the upper part of the esophagus. This type is becoming less common among Americans. Around the world, however, squamous cell carcinoma is the most common type.
Treatment : There are several types of surgery for esophageal cancer. The type depends mainly on where the cancer is located. The surgeon may remove the whole esophagus or only the part that has the cancer. Usually, the surgeon removes the section of the esophagus with the cancer, lymph nodes, and nearby soft tissues. Part or all of the stomach may also be removed. You and your surgeon can talk about the types of surgery and which may be right for you.
The surgeon makes incisions into your chest and abdomen to remove the cancer. In most cases, the surgeon pulls up the stomach and joins it to the remaining part of the esophagus. Or a piece of intestine may be used to connect the stomach to the remaining part of the esophagus. The surgeon may use either a piece of small intestine or large intestine. If the stomach was removed, a piece of intestine is used to join the remaining part of the esophagus to the small intestine.
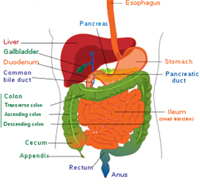 The bowel is a muscular tube extending from the mouth to the anus. Cells that provide complete protection to the tissues forming the wall of the bowel line its interior. Any break in this lining is known as an ulcer. When ulcers occur in the gut, they are more likely in two main places, in the stomach and in the duodenum (the part of the small bowel immediately the stomach). An ulcer in the stomach is known as a gastric ulcer, and one in the duodenum is referred to as a duodenal ulcer. For reasons discussed below, gastric and duodenal ulcers are also called peptic ulcers.
The bowel is a muscular tube extending from the mouth to the anus. Cells that provide complete protection to the tissues forming the wall of the bowel line its interior. Any break in this lining is known as an ulcer. When ulcers occur in the gut, they are more likely in two main places, in the stomach and in the duodenum (the part of the small bowel immediately the stomach). An ulcer in the stomach is known as a gastric ulcer, and one in the duodenum is referred to as a duodenal ulcer. For reasons discussed below, gastric and duodenal ulcers are also called peptic ulcers.
The stomach produces hydrochloric acid and an enzyme called pepsin, and the two
begin the process of digestion of food. These substances are so powerful that they can
easily digest the lining and wall of the stomach, but the reason they do not is because
there are equally powerful defence mechanisms that protect the lining of the bowel.
Ulcers occur when the defences of the bowel lining are overcome by acid and pepsin,
and the lining is eaten away to leave a raw patch.
These ulcers are named 'peptic'
because pepsin is one of the corroding substances. Ulcers do not form if there is no
acid, but people with ulcers do not necessarily produce more acid in their stomachs
than people without ulcers. In those with ulcers, however, reducing acid production
increases the chances of the ulcers healing.
A germ or bug called Helicobacter pylori (or H. pylori) has now been identified as an important cause of peptic ulcers. Nearly all patients with duodenal ulcer have it, and 80% of those with gastric ulcer have this bug.
Anyone can get peptic ulcers, but they are more common in younger adults. Men get ulcers more than women. Factors that increase the risk of ulcers include:
- Cigarette smoking
- The use of medicines known as non-steroidal anti-inflammatory drugs, for treatingarthritis and rheumatism
- The use of steroids, also for treating certain forms of rheumatism and arthritis
- Excessive alcohol
- Stress by itself does not produce ulcers but aggravates them if they already exist.There is no evidence that eating spicy foods causes ulcers.
If you have pain in the tummy that fits into one or more of the following categories:
- Usually felt in the upper part of the middle of the tummy
- Sometimes goes straight through into the back
- Is burning in character and wakes you up in the middle of the night
- Sometimes occurs when you are hungry and is better after you drink milk
- Some types of peptic ulcers are made worse by food
- May be accompanied by nausea and occasionally vomiting
- If you develop complications such as vomiting blood
The two main ones are barium meal and gastroscopy . Gastroscopy is preferred nowadays as it enables tissue samples to be taken to rule out cancer and to determine whether H. pylori is present.
There are a number of ways of treating ulcers but always make sure that treatment is recommended and supervised by your doctor:
- Avoiding altogether or reducing the things that caused them or those making them worse, eg excessive alcohol, smoking, steroids and non-steroidal antiinflammatory drugs and stress
- Avoiding foods that aggravate them and eating small and frequent meals toneutralise stomach acid. It is not necessary to eat just bland foods.
- Reducing stomach acid. This involves the use of simple antacids or medicines that specifically block the cells that produce acid. There are a number of these on the market, some obtainable over the counter.
- Eradicating H. pylori if present. Your doctor will recommend a combination of antibiotics and an acid suppressing medication for a week or two.
- Using medications that strengthen the lining of the stomach and prevent its damage
Fortunately with all the medicines now available, it is uncommon for surgeons to
operate on peptic ulcers. Operations were done to cut the nerves supplying the acid
producing cells or removing a portion of the stomach. Operations are still necessary
when complications such as bleeding or perforation of the stomach occur.
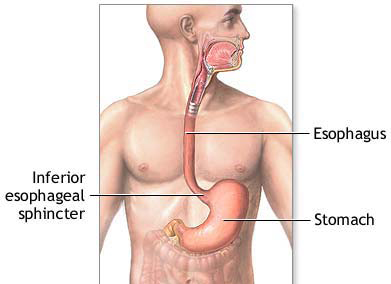
Hiatus hernia is a condition in which the upper part of the stomach is pushed up into the lower part of the chest through a weakness in the diaphragm. The diaphragm is a strong, dome-shaped sheet of muscle that separates the chest from the abdominal cavity. The oesophagus or gullet passes through the diaphragm on its way to join the stomach, which lies immediately on its underside. In some people, the opening through which the oesophagus passes becomes slack and allows the top part of the stomach to rise into the chest.
Many people have hiatus hernias that do not cause any symptoms and are discovered entirely by chance during x-rays or endoscopy examinations of this area. No action needs to be taken for such a hernia. Symptoms caused by hiatus hernia are due to the juices from the stomach working their way upwards and eroding the lining of the gullet. This is referred to as gastro-oesophageal reflux. The lining of the gullet was not designed to come in contact with gastric juices. The lining is inflamed and eroded (reflux oesophagitis), resulting in heartburn . The symptoms are made worse if the individual is overweight, wears tight clothing such as abdominal corsets, or bends down often or lies flat in bed. These symptoms also occur in pregnant women but often clear after the baby is born.
A more serious problem due to the constant irritation of the lining of the gullet is the formation of scar tissue in the gullet leading to narrowing of the gullet. If this is not relieved the individual will have difficulty in swallowing and this can itself lead to many complications.
The pain of hiatus hernia can sometimes mimic heart disease and so it is important to establish the diagnosis with certainty. Your doctor, on listening to your history and examining you will decide on the tests to perform to make a diagnosis. These will include doing a heart tracing or ECG, a barium meal and/or oesophago-gastroduodenoscopy. During the last tests, biopsies can be taken to determine the extent of inflammation of the oesophagus. These tests will also determine the degree of narrowing of the oesophagus.
The treatment in most people is by simple means, supplemented by medications.
- Having small but frequent meals. Have drinks at different times to meals.
- Avoid foods which may cause problems, mainly spicy, fatty or fried foods, strong coffee, fizzy drinks, lots of caffeine, alcohol, very hot or very cold drinks
- Adopt better posture. Avoid bending, lifting and lying down for 2 hours after food. Cut down on or give up smoking.
- Tight fitting clothes and underwear can sometimes aggravate the problem.
- If you suffer badly at night, try sleeping with extra pillows; alternatively, you can prop up the bed a few inches at the head end.
- Milk and yoghurt may help to relieve the symptoms.
- If you are overweight, it is important to lose weight, as this may alleviate most of your symptoms.
- Your doctor will prescribe medications that help to neutralise the acid coming upinto the gullet, to reduce acid production and to help the gullet to empty the acid that comes into it more quickly. A number of these medications are now available
on the market and some can be bought over the counter at chemists. It is important not to treat yourself but to follow treatment prescribed by the doctor.
In most people, symptoms are controlled by the measures above. An operation is considered in the minority of patients in the following categories: those in whom symptoms control is ineffective by these means; those who have dangerous bleeding from the gullet due to the damage by the acid; those who have narrowing of the gullet and have difficulty swallowing.
The aim of the operation is to get the stomach back into the abdominal cavity, to reduce the size of the hole in the diaphragm so the stomach cannot slip back upwards, and to restore the valve mechanism to stop acid going up into the gullet. Several
operations have been tried and many abandoned as they were not very effective or were deemed dangerous. They all involved cutting through the abdominal wall to reach the gullet, and then performing the repair.
The new way is to use the laparoscope or the key-hole technique, and the operation is called laparoscopic fundoplication. The stomach is brought down and a part of it wrapped around the lower gullet to achieve the aims above. Recovery is quick and in good hands the results are very promising.
If the gullet has become narrowed, it can now be easily stretched or dilated using a gastroscope. This stretching, often a day case procedure, needs to be repeated several times under sedation. Rarely, it may be necessary to leave a tube permanently in the gullet to keep it open but this is very rarely done for this particular problem.

Laparoscopic Trichobezoar Removal
The stomach is a hollow organ in the upper abdomen, under the ribs.
It's part of the digestive system. Food moves from the mouth through the esophagus to the stomach. In the stomach, the food becomes liquid. Muscles in the stomach wall push the liquid into the small intestine.
Studies have found the following risk factors for stomach cancer:
Helicobacter pylori infection: H. pylori is a bacterium that commonly infects the inner lining (the mucosa) of the stomach. Infection with H. pylori can cause stomach inflammation and peptic ulcers. It also increases the risk of stomach cancer, but only a small number of infected people develop stomach cancer.
Long-term inflammation of the stomach: People who have conditions associated with long-term stomach inflammation (such as the blood disease pernicious anemia) are at increased risk of stomach cancer. Also, people who have had part of their stomach removed may have long-term stomach inflammation and increased risk of stomach cancer many years after their surgery.
Smoking: Smokers are more likely than nonsmokers to develop stomach cancer. Heavy smokers are most at risk.
Family history: Close relatives (parents, brothers, sisters, or children) of a person with a history of stomach cancer are somewhat more likely to develop the disease themselves. If many close relatives have a history of stomach cancer, the risk is even greater.
The type of surgery for stomach cancer depends mainly on where the cancer is located. The surgeon may remove the whole stomach or only the part that has the cancer.You and your surgeon can talk about the types of surgery and which may be right for you:
Partial (subtotal) gastrectomy for tumors at the lower part of the stomach: The surgeon removes the lower part of the stomach with the cancer. The surgeon attaches the remaining part of the stomach to the intestine. Nearby lymph nodes and other tissues may also be removed.
Total gastrectomy for tumors at the upper part of the stomach: The surgeon removes the entire stomach, nearby lymph nodes, parts of the esophagus and small intestine, and other tissues near the tumor. Rarely, the spleen also may be removed. The surgeon then connects the esophagus directly to the small intestine.


.jpg)